Electronic Real-Time Claim Status (EDI 276/277)
Electronic Real-Time Claim Status
One of the pain points for billing professionals is to monitor submitted claims. It is reported that when a provider manually runs a claim status check, on average it takes 19 minutes and costs providers $9.37. In 2020, providers made 238 million claim status inquiries by phone, fax, or email. Most payers still limit the number of inquiries allowed per call, which means more calls, more work for staff and more time wasted. And that’s before adding in the time it takes to update claim statuses in practice management (PM) or hospital information systems (HIS). To unlock the cost savings and smarter workflows they need, it’s critical to deploy the electronic real-time claim status check and post the status in a practice management system that can easily automate the process.
MDOS Billing Pro real-time claim status checking services for several commercial payers (Aetna, Cigna, Humana, United HealthCare, and others) to help providers streamline their reimbursement process. Claim status results are immediate, easy to read, and contain important adjudication information. These services will allow you to determine whether a claim sent was accepted, rejected, or pending at the payer. It offers the ability to review any available adjudication/payment information. No more waiting on hold with a payer or dealing with automated IVR phone systems to check on claim status; saving you time and money.
Combined with ERA (The electronic EOB), while ERA (Electronic Remittance Advice) posting tracks the insurance payments of the majority of claims, the real-time claims status check takes care of the rest, and more time will be saved to monitor and check healthcare claim status in the revenue cycle.
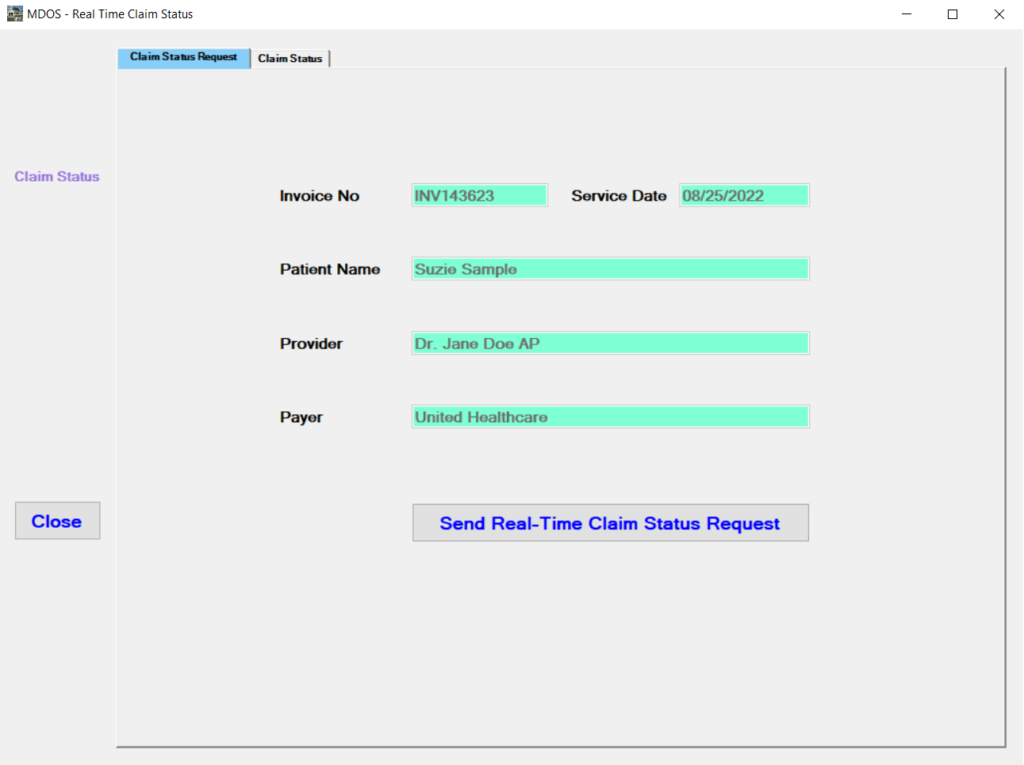
Claim Status Request
An electronic inquiry from a provider to a health plan to determine the status of a health care claim only takes a few seconds, greatly reducing labor costs related to the long phone calls, error-prone manual verification and recording, and workflows. Specifically, it takes 19 minutes to check a claim status manually and it takes a few seconds to check a claim status electronically; It costs $9.37 to check a claim status manually and it costs $10.00 to check 100 claim status electronically. The benefits of electronic real-time claim status check and auto-posting claim status are:
- Eliminate manual keying; save time and effort
- Reduce posting errors
- Increase efficiency and save money
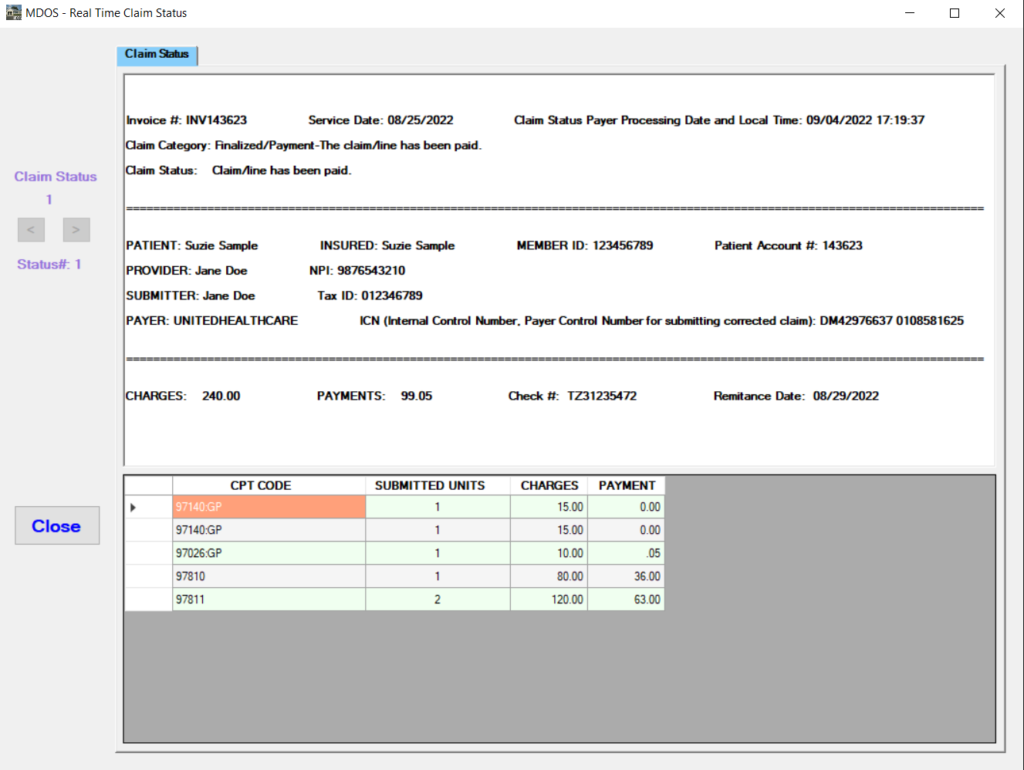
Claim Status Response
A response from the health plan to a provider about the status of a health care claim includes the following, which is saved into the MDOS system automatically and can be viewed at a later time.
- Claim Invoice Number
- Service Date
- Category Description
- Status Description
- Patient Insurance Member ID
- Patient Account Number
- Provider Name and NPI
- Submitter Name and Tax ID
- Payer’s Claim Control Number
- Claim Charge Amount
- Claim Payment Amount
- Check Number
- Remittance Date
- Procedure Code
- Procedure Units
- Procedure Charges
- Procedure Payments